
This 35 question renal quiz is designed for medical students and covers key concepts in kidney structure, function, and pathophysiology. As always, you can answer anonymously, with immediate feedback, and can try again as often as you like.

This 35 question renal quiz is designed for medical students and covers key concepts in kidney structure, function, and pathophysiology. As always, you can answer anonymously, with immediate feedback, and can try again as often as you like.
👩⚕️ Meet Karen, a 54-year-old woman with Type 2 Diabetes and longstanding hypertension. She’s noticed some ankle swelling, increasing fatigue, and mild nausea. Her GP runs bloods— her eGFR is 38 mL/min/1.73m², her creatinine is up, and there’s proteinuria.
Beneath those swelling ankles lies a story of pressure, filtration failure, and systemic fallout. This is where physiology meets clinical reality, and small changes start to snowball.
Renal function tests aren’t just numbers — they’re clues. When interpreted thoughtfully, they can help us distinguish between dehydration, intrinsic renal disease, and post-renal obstruction. In this post, you’ll meet patients like Tom, who presents with dehydration and rising creatinine; Aisha, whose frothy urine holds a glomerular secret; and Leo, whose “normal” labs conceal a chronic decline — all to help you decode renal results with clinical confidence.
We’ll explore how to interpret renal function tests and urinalysis through a clinical reasoning lens — breaking down key blood and urine markers, comparing patterns across different types of kidney injury, and working through real-world cases to bring the concepts to life.
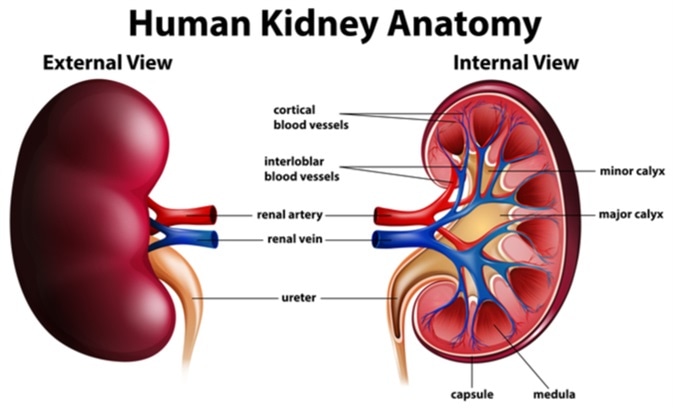
The kidney is not merely a blood-cleaning organ — it’s a precisely engineered filtration system, packed into a space smaller than your fist. At the heart of this system lies the glomerulus, a tight ball of capillaries ensconced within Bowman’s capsule, where blood meets filter.
When this filter becomes inflamed — a condition called glomerulonephritis
(GN) — its normally selective barrier becomes leaky, irritable, and
dysfunctional. Blood cells and proteins that should stay in the bloodstream
escape into the urine. Waste products that should be cleared begin to build up.

In this post, we’ll explore what glomerulonephritis actually is, how it disrupts the kidney’s filtration barrier, and why understanding its immune mechanisms matters — especially before diving into clinical patterns.
🧭 Coming Up after this in Part 2, we’ll explore how these injuries translate into clinical syndromes — particularly the classic nephritic vs nephrotic divide — and walk through real-world cases to bring the concepts to life.
 A 12-question quiz on urinary tract infections and pyelonephritis, focusing on microbiology, pathophysiology, antibiotic choice, and host defences.
A 12-question quiz on urinary tract infections and pyelonephritis, focusing on microbiology, pathophysiology, antibiotic choice, and host defences.
Infections in the renal system are among the most common reasons patients present to GPs and emergency departments — yet their underlying mechanisms are often oversimplified. These aren't just “bladder bugs” causing discomfort: they are dynamic, evolving conditions that reflect an interplay between microbial virulence, host defence, and anatomical vulnerabilities.
From the relatively straightforward presentation of cystitis to the more serious implications of pyelonephritis, renal infections provide a perfect lens through which to explore the clinical relevance of physiology and pathophysiology. How does a bacterium from the gut end up damaging a kidney? What determines whether a simple UTI becomes a systemic illness? And how do we decide when antibiotics, imaging, or hospital admission are truly necessary?
In this post, we’ll explore how renal infections arise, what differentiates upper from lower tract involvement, and how pathophysiological principles guide investigation and treatment decisions.
A 10-question quiz on renal physiology and blood pressure regulation, focusing on RAAS, nephron function, sympathetic tone, and antihypertensive drug mechanisms.
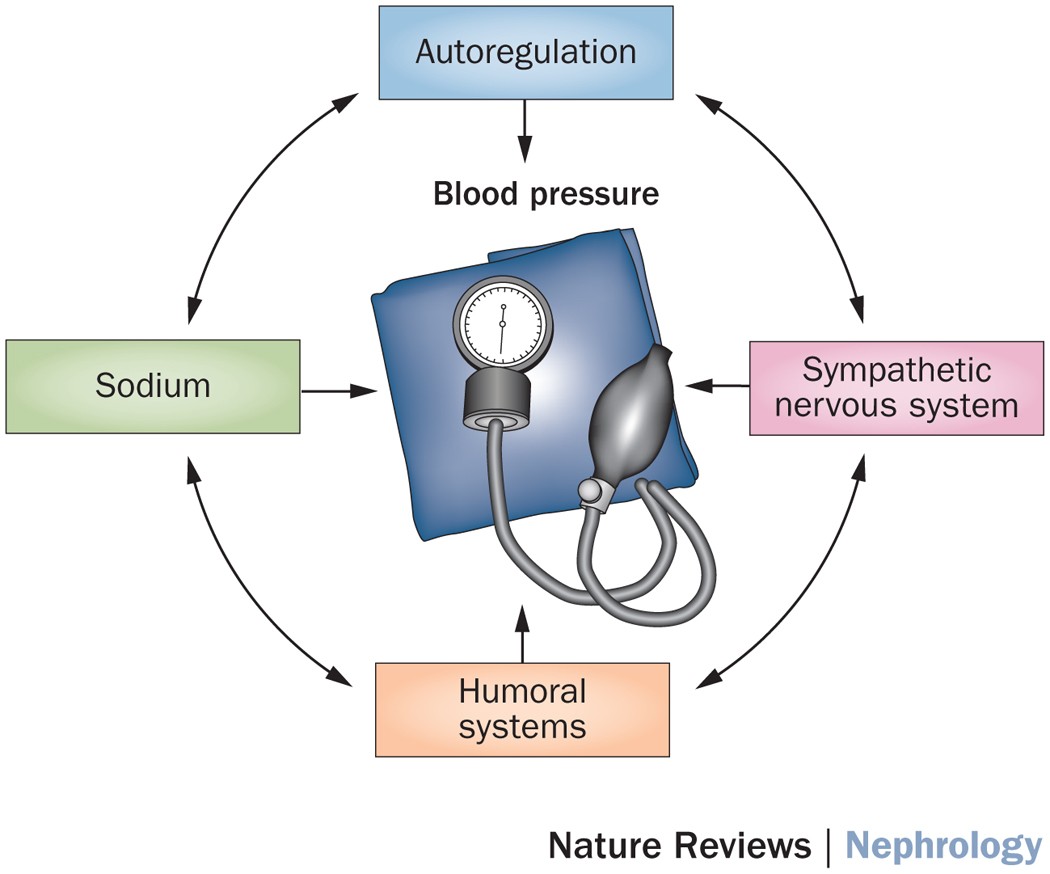
The kidneys are best known for filtering waste and producing urine — but they are also key regulators of long-term blood pressure. Far from passive filters, they act as fluid managers and hormonal sensors, constantly monitoring blood flow, volume, and salt levels, then adjusting the body's internal settings to stabilise the circulation.
The cardiovascular system doesn’t operate in isolation — it
relies on input from other organs, and the kidneys are among the most
influential. Through a combination of neural and hormonal feedback, they
help maintain vascular tone and circulating volume. This role becomes
especially apparent in chronic conditions such as hypertension and chronic
kidney disease, where blood pressure control and renal function often
deteriorate together.
Many commonly used antihypertensives — including diuretics,
ACE inhibitors, and angiotensin receptor blockers — work by targeting renal
processes or the hormones the kidney influences. Understanding how the
kidneys detect and respond to systemic signals forms the foundation not
only for renal physiology, but for clinical reasoning in cardiovascular disease
and pharmacological management.
In this post, we’ll explore how the kidneys sense and
respond to changes in blood pressure — and how this underpins both disease
processes like hypertension and the mechanism of action for many
antihypertensive drugs.
Test your understanding of core medical concepts across systems! This 40-question quiz is packed with clinical vignettes and applied physiology from topics like asthma, digestion, gas exchange, renal handling, antibiotics, ECGs, liver disease, pharmacology and more. Can you get through the full set?
 Test your understanding of nephron structure and kidney physiology with these five quiz questions.
Test your understanding of nephron structure and kidney physiology with these five quiz questions.
A 56-year-old woman visits her GP with two common but vague symptoms: fatigue and ankle swelling. Her vitals and labs show:
As a GP, I'd be asking: are these early signs of chronic kidney disease (CKD), or part of a broader hypertensive picture? These results might seem only mildly abnormal, but even “moderate” kidney dysfunction can signal serious shifts in physiology. So—what’s failing? And why do those failures affect more than just the urine?
This post walks through how each part of the nephron contributes to health, and what happens when that function begins to slip.
 A 5-question quiz exploring the pathophysiology of alcohol-related and non-alcoholic fatty liver disease (ARLD vs NAFLD). Read each clinical scenario and choose the best explanation.
A 5-question quiz exploring the pathophysiology of alcohol-related and non-alcoholic fatty liver disease (ARLD vs NAFLD). Read each clinical scenario and choose the best explanation.
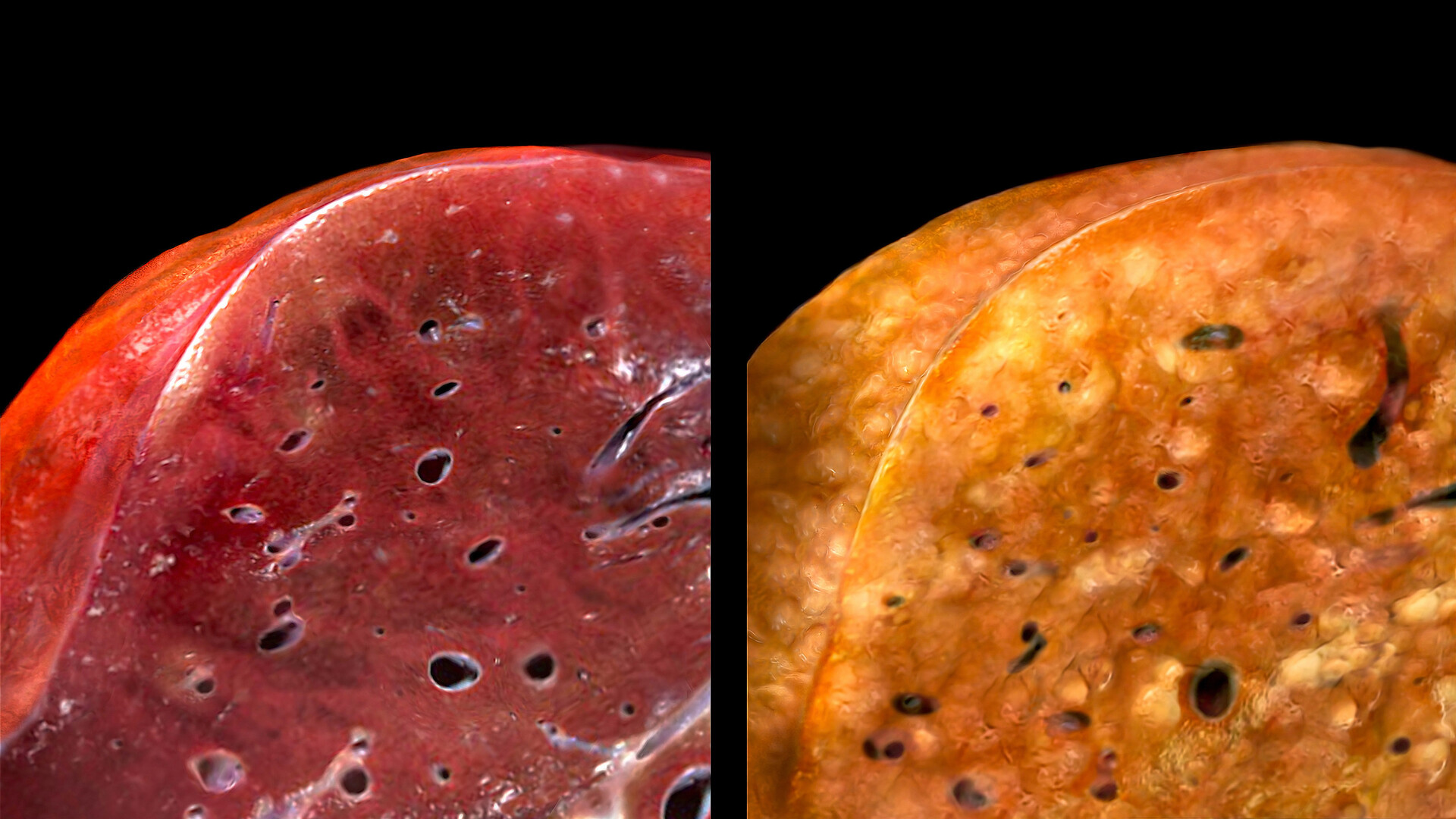
In this post, we explore the similarities and differences between alcohol-related liver disease (ARLD) and non-alcoholic fatty liver disease (NAFLD)—two of the most common causes of liver dysfunction worldwide.
Both progress through similar pathological stages but have distinct
triggers, mechanisms, and associated conditions. Let’s dive into how each
affects liver structure and function.
Test your understanding of Hepatitis B serology with these five clinical scenarios. Can you apply serological markers to real-world cases?
I'm very pleased to share our latest publication in BMC Medical Education: "Medical school admission processes to target rural applicants: an international scoping review and mapping of Australian practices."
https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-025-07234-3
Alongside esteemed colleagues from Deakin University, Charles Sturt University, University of Queensland, University of Melbourne, University of Adelaide, Western Sydney University, and the University of South Australia, we explored how Australian medical schools select rural applicants.
Our findings reinforce the importance of recruiting rural-origin students to address workforce shortages, revealing significant variations in how academic performance metrics and standardised tests are weighted across institutions. While many medical schools adapt entry criteria for rural candidates, greater consistency and evidence-based approaches could improve fairness and long-term healthcare sustainability.
This research aligns with international studies supporting tailored admission processes to strengthen rural health outcomes. We advocate for modified pathways that ensure equitable access to medical education and a stronger rural medical workforce.
Test your knowledge of chronic viral hepatitis, liver fibrosis, and hepatocellular carcinoma using these best-of-five questions designed to reinforce key clinical and pathophysiological concepts.
While many patients recover completely from an episode of acute hepatitis, certain hepatitis viruses—especially Hepatitis B (HBV) and Hepatitis C (HCV)—fail to be cleared from the body. This persistence triggers a continuous inflammatory cascade in the liver, laying the groundwork for progressive scarring and, eventually, the development of hepatocellular carcinoma (HCC).
These Best-of-Five questions will test your understanding of the pathophysiology, transmission, and laboratory features of acute viral hepatitis. Ready to apply what you've learned? Like all the quizzes, you can have a try and check your answers anonymously, then reset the quiz to try again later !
Acute viral hepatitis refers to sudden-onset liver inflammation caused by one of the hepatitis viruses — most commonly Hepatitis A, B, C, D, or E. Each virus has distinct routes of transmission, clinical behaviour, and implications for public health — but they share overlapping patterns of hepatic injury.
In this post, we will explore:
🩺 Quiz: Signs of liver dysfunction

Test your understanding of liver function and its role in metabolism, clotting, bilirubin clearance, and neurological complications. Choose the best answer for each case, then check your score and explanations.
The liver is essential for metabolism, synthesis, detoxification, immune regulation, and storage. When liver function fails, distinct signs emerge—often across multiple systems.
This guide explains why these signs occur and how they relate to underlying liver dysfunction. Rather than trying to memorise a list of signs - it is always better to think pathophysiologically from first principles- then you will know HOW and WHY things happen as they do.
This five-question quiz helps medical students review key concepts in liver structure, dual blood supply, bile flow, and complications of liver dysfunction such as jaundice, coagulopathy, and encephalopathy.
The liver is a multitasking marvel. Few organs work harder than the liver. Whether it’s keeping blood clotting smoothly, neutralising toxins, or managing energy reserves, its failure can lead to striking clinical signs—some subtle, others life-threatening. Weighing just under 1.5 kg, it constitutes about 2% of an adult’s body weight but contributes to hundreds of critical biochemical processes. It is your metabolic hub, your detox centre, your protein factory, and your immune gatekeeper — all in one. Despite its resilience, even minor dysfunction can throw multiple systems off balance—making liver disease a key challenge in medicine.
Understanding its structure and function will help explain why liver dysfunction produces such distinct clinical signs.