👋 Let’s dive into the fascinating (and complex) world of Rheumatoid Arthritis (RA)—a classic autoimmune disorder that’s important to understand for future clinical practice. 🩺📚
Monday, 10 November 2025
Rheumatoid Arthritis: Unravelling the Pathophysiology 🧬
Thursday, 6 November 2025
Antiphospholipid syndrome: A prothrombotic puzzle
Pathophysiology of antiphospholipid syndrome
Antiphospholipid syndrome (APS) is an autoimmune disorder characterised by the presence of antiphospholipid antibodies (aPL), which target phospholipid-binding proteins involved in coagulation. These antibodies disrupt normal endothelial function, leading to hypercoagulability and an increased risk of thrombosis.
Wednesday, 5 November 2025
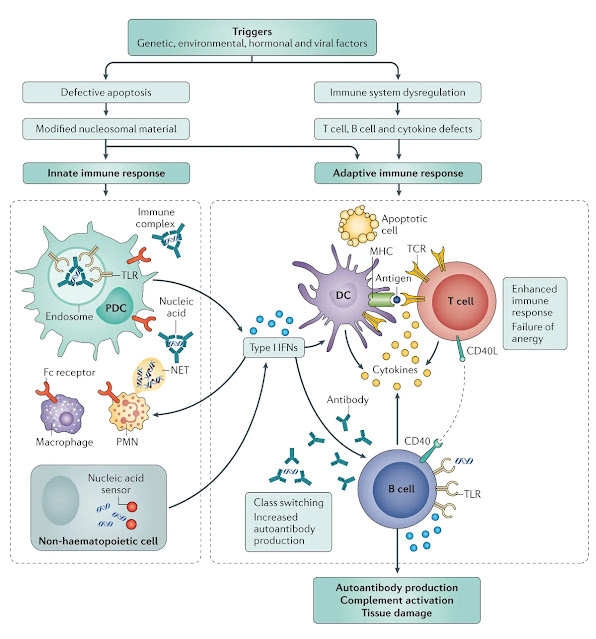
Understanding the pathophysiology of systemic lupus erythematosus (SLE)
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease characterised by multisystem involvement and a complex interplay of genetic, environmental, and immunological factors. It primarily affects young women and can manifest with diverse clinical symptoms, ranging from mild cutaneous involvement to life-threatening organ damage. Understanding its pathophysiology is crucial for developing targeted therapies and improving patient outcomes.
Tuesday, 4 November 2025
Immune Tolerance & The Development of Autoimmunity
The immune system functions as a highly selective defence network, recognising foreign pathogens while preserving self-tolerance to avoid attacking the body’s own tissues. This balance is essential for immune homeostasis—but when tolerance mechanisms break down, autoimmune diseases develop, causing chronic inflammation and tissue destruction.
Understanding how immune tolerance is established, maintained, and eventually fails provides critical insight into the pathophysiology of autoimmunity.
Saturday, 11 October 2025
🧠 The Gonadal axis - Part 2 : Male physiology
In males, the HPG axis governs testicular development, spermatogenesis, and testosterone production. These processes begin in foetal life, pause in childhood, and reactivate at puberty — shaping not only fertility, but muscle mass, libido, voice, and bone health.
Understanding normal male physiology is essential before exploring disorders like hypogonadism, delayed puberty, or infertility.
🧠 The Gonadal Axis — Part 1 - Normal Physiology Across the Lifespan
The Hypothalamic–Pituitary–Gonadal (HPG) axis governs the development and regulation of reproductive physiology, including puberty, gametogenesis, menstrual cycles, and sexual function. It’s a dynamic system that responds to internal cues (like age and energy availability) and external signals (like stress and illness).
Its activity varies dramatically across the lifespan, from foetal differentiation to puberty, reproductive maturity, and eventual decline. Understanding this baseline physiology is essential before exploring disorders of puberty, fertility, or sexual function.
Friday, 10 October 2025
ECG Interpretation: A Reasoning-Based Revision Guide 🫀
Interpreting an ECG isn’t just about spotting abnormalities — it’s about understanding the heart’s electrical story in the context of the patient. This guide breaks down the process step by step.
If you need a reminder of the electrophysiology of the heart you can find that here
Tuesday, 7 October 2025
🧠 The Growth Axis - Part 2 : Famous faces of endocrinology
Robert Wadlow — Tallest man in history
Robert Pershing Wadlow (1918–1940), known as the “Alton Giant,” holds the record as the tallest verified human in history. He reached a height of 2.72 m (8'11") and weighed over 220 kg at the time of his death — the result of uncontrolled growth hormone excess due to a pituitary adenoma.
🧠 The Growth Axis - Part 1 : physiology and disorders of height and growth
Growth isn’t just about getting taller, it’s about coordinated development across tissues, organs, and systems. The hypothalamic-pituitary-somatomedin (HPS) axis governs this process, linking brain signals to liver output and peripheral tissue response. It’s a slow axis, but a powerful one - and when it fails, the consequences are lifelong.
Monday, 6 October 2025
🧠 The Adrenal Axis - Adrenal insufficiency, Cushing's syndrome and Adrenal crisis.
The hypothalamic-pituitary-adrenal (HPA) axis is your body’s central stress-response system. It’s not just about cortisol, it’s about how the brain, pituitary, and adrenal glands coordinate to keep you alive under pressure. Whether you’re managing infection, trauma, or emotional strain, the HPA axis is quietly adjusting your metabolism, blood pressure, and immune response.
Ten patients: clinical cases in endocrinology - the thyroid axis
The thyroid axis is a finely tuned system that regulates metabolism, growth, and energy balance. Disturbances in this axis can present subtly or dramatically, and understanding them requires more than memorizing hormone levels, it demands clinical reasoning.
In the following 10 cases, you’ll explore a spectrum of thyroid dysfunctions, from common presentations to critical emergencies.
🔍 Common Causes of Hypothyroidism: Hashimoto's thyroiditis
Hashimoto’s thyroiditis is the most common cause of hypothyroidism in iodine-sufficient regions — and a classic example of destructive autoimmunity. Unlike Graves’ disease, which stimulates the thyroid, Hashimoto’s gradually damages and disables it. The immune system mistakes thyroid tissue for a threat, and over time, hormone production declines.
This post will walk you through:
- How the immune system targets the thyroid
- What antibodies and histology reveal
- How to reason through the progression from normal to low hormone states
- What to look for on imaging
- How to manage the condition clinically
🔺 Pathophysiology of HYPOthyroidism
In the last few posts, we explored what happens when thyroid hormone levels are too high and how Graves’ disease, toxic nodules, and thyroiditis each disrupt the HPT axis in different ways. Now we turn to the opposite problem: hypothyroidism.
What happens when there’s not enough thyroid hormone in the
body?
Unlike hyperthyroidism, where everything speeds up,
hypothyroidism causes a gradual slowing of metabolic processes across multiple
systems. Patients may feel tired, cold, constipated, and foggy - but these
symptoms often creep in slowly, and are easy to miss unless you understand the
underlying physiology.
Thyroid hormone (especially T3) acts as a metabolic accelerator. It increases mitochondrial activity, oxygen consumption, and protein turnover. It also sensitises tissues to catecholamines, regulates lipid and carbohydrate metabolism, and supports normal growth and development. So when levels fall, the whole system downshifts.
Sunday, 5 October 2025
🔍 Common Causes of Hyperthyroidism: Graves’ Disease, Toxic Multinodular Goitre, and Thyroiditis
In the last post, we explored what happens when thyroid hormone levels are too high — and how to reason through the possible causes using the HPT axis. Now, we turn our focus to the three most common conditions that medical students are likely to encounter in practice: Graves’ disease, toxic multinodular goitre (TMNG), and thyroiditis.
These conditions may all present with elevated T3 and T4,
but they arise from fundamentally different mechanisms (autoimmune
stimulation, nodular autonomy, and inflammatory leakage) and require very
different approaches to diagnosis and management.
In this post, we’ll walk through each condition in detail,
exploring the pathophysiology, clinical features, investigations, and reasoning
that help distinguish them. By the end, you’ll be able to interpret thyroid
function tests, understand scan results in context, and explain
to patients why their thyroid is misbehaving !
🔺 Pathophysiology of HYPERthyroidism
What happens when there’s too much thyroid hormone in the body?
When thyroid hormone levels are elevated, the body doesn’t
just “speed up”, it becomes overstimulated across multiple systems. This isn’t
a random collection of symptoms; it’s a predictable physiological response to
excess T3 and T4.
Saturday, 4 October 2025
🧠 The Thyroid Axis
The thyroid axis is one of the most common clinically encountered endocrine systems. It regulates metabolism, temperature, energy, and mood. Understanding how it works helps you reason through symptoms like fatigue, weight change, palpitations, constipation, and menstrual irregularities.
🧠 The Hypothalamic–Pituitary Axis: Physiology, Reasoning, and Clinical Relevance
Welcome to endocrine! This post is designed to help you reason through the hypothalamic–pituitary axis (HPA), not just memorise it. You don’t need to know everything yet. What matters is understanding how the system works, how it regulates itself, and how that explains common clinical presentations.
Thursday, 2 October 2025
Preparing for exams - how to make the next two months work best for you
Exams are just under eight weeks away - close enough to feel real, but still enough time to prepare steadily without panic. The key now is consistency. Small, regular efforts will carry you much further than bursts of late-night cramming.
This post pulls together some evidence-based strategies, links back to resources you already have, and sets out how you can use the coming weeks to your advantage.
Tuesday, 30 September 2025
Surgeons Outside of Cities: New Research from UOW GSM
We’re proud to celebrate Dr Tracey Edwards, UOW Medicine Class of 2023, whose latest article has just been published in the Australian Journal of Rural Health.
📖 Read the full open-access article here: Surgeons Outside of Cities – AJRH 2025
Key findings from the research include:
-
The total number of surgeons in Australia rose from 4,568 to 5,724 across the decade.
-
Only 15.5% of surgeons now practise in rural areas (down from 16.9% in 2013), despite 29% of Australians living outside metropolitan centres.
-
Female surgeons remain under-represented, particularly in rural settings (12.4%), with the paper noting barriers such as long hours, lack of mentoring, and family/partner considerations.
-
Surgical sub-specialties other than general surgery are rare in regional and rural Australia.
This work highlights both progress and persistent challenges in ensuring equitable surgical care for all Australians. It underscores the importance of initiatives to attract and retain surgeons in regional and rural practice, including targeted training, mentoring, and support for women in surgery.
Thursday, 25 September 2025
Why “High Yield” Thinking is Harmful in Medicine
You may hear medical students talk about “high yield” and “low yield” topics, the idea that some things are worth learning because they’ll score marks, while others can safely be ignored. I, like many others, find this discussion at best irritating and at worst exasperating or even offensive. Why?
This mindset is short-sighted and demeaning to patients and their experiences. Labelling parts of the curriculum as “low yield” suggests they are less valuable, when in reality, every condition, system, and clinical story matters to the people living it. The “rare” syndrome, the “niche” complication, or the “uncommon” presentation may be the defining moment in one patient’s life - and the patient in front of you deserves your full attention, not a calculation of yield.There is also a degree of arrogance in the “high yield”
mindset. As students, you do not yet have the experience to judge what will or
won’t be important in your future practice. What feels irrelevant today may be critical tomorrow. Senior medical educators have
designed the curriculum with decades of accumulated wisdom. To dismiss parts of
it as “low yield” is to assume you know better than those who have seen the
consequences when knowledge gaps harm patients.
Focusing only on what might appear in exams encourages
skipping over knowledge simply because it’s uncommon, uninteresting to you, or because you don't yet have the experience to understand its value. That erodes your future
readiness as a doctor and risks patient safety. Medicine is built on breadth as
well as depth - on curiosity, humility, and a willingness to take every
presentation seriously. You don’t get to choose which patient walks through
your door. When it’s their story, it will always be high yield.
Instead of chasing the most marks for the least effort, or
trying to be “strategic,” aim higher: focus on becoming the best doctor you can
be. That means:
- Building
strong foundational concepts that you can apply across conditions.
- Seeking
integration: understanding how systems connect, not just isolated
facts.
- Practising
clinical reasoning: applying knowledge in scenarios, not memorising
lists.
- Reflecting
on the kind of doctor you want to be - one who values marks, or one
who values patients.
Exams will come and go, but your patients will live with the
consequences of how seriously you approached your learning. Choose to respect
the curriculum, respect your educators, and above all respect your
patients - because in real medicine, everything is high yield.
Sunday, 31 August 2025
Understanding common fracture types 🦴
Saturday, 30 August 2025
Osteoporosis: The Silent Thief of Bone 🦴
Hey students! 👋 Let’s take a deep dive into osteoporosis—a condition that’s far more than just “brittle bones.” In Australia, 1 in 3 women and 1 in 5 men over 50 will experience an osteoporotic fracture.
Understanding, investigating and managing pericarditis
You’ll hear it described as “sharp chest pain,” “worse when lying flat,” or “relieved by sitting forward.” But what’s actually happening when someone has pericarditis—and how do we reason through it clinically?
Let’s explore the pathophysiology first, then walk through how to spot it, investigate it, and manage it.
Tuesday, 19 August 2025
🧠 Psychosis or delirium : a complex interplay
Acute physical illness doesn’t just affect the body - it can destabilize the mind. For patients with schizophrenia, dementia or other psychotic or neurodegenerative disorders, infections like pneumonia or urinary tract infections can trigger agitation, paranoia, or hallucinations.
Understanding this interplay is essential for safe, compassionate care in hospital settings.
Lower Limb Anatomy in Motion: Structure Meets Function
Every time you take a step, shift your weight, or rise from a chair, your body performs a complex, coordinated dance. The lower limb and pelvis aren’t just anatomical regions—they’re the foundation of mobility, balance, and independence. For older adults, even subtle disruptions in this system can lead to instability, falls, and fractures. Understanding how these structures work together—and what happens when they fail—is essential for building clinical reasoning from day one.
Let’s explore how bones, joints, muscles, and connective tissues work together to keep you upright—and what happens when they don’t.
Falls in the Elderly: A Preventable Problem
Falls are a major cause of injury and loss of independence in older adults. In Australia, 1 in 3 people over 65 will experience a fall each year—and for many, it’s a life-changing event.
But here’s the good news: most falls are preventable. This post explores the why, how, and what you can do about it.
Monday, 18 August 2025
Hip Fractures: A Major Challenge in Ageing Populations 🦴
Let’s talk about hip fractures—a serious and often life-altering injury, especially for our elderly patients. In Australia, hip fractures are one of the leading causes of hospital admissions in people over 65. They’re not just painful—they’re a sentinel event, often marking a turning point in a patient’s independence, mobility, and overall health.
But what exactly is a “hip fracture”? And why does it carry such weight in clinical practice?
The Normal Physiology of Bone: Remodelling, Healing & Influencing Factors 🦴
Bone physiology might seem like a dry topic at first glance, but it’s anything but. It’s the key to understanding how fractures heal, why osteoporosis develops, and what goes wrong in metabolic bone diseases. For future clinicians, this knowledge isn’t just theoretical—it’s the basis for diagnosing, managing, and preventing some of the most common and impactful conditions you’ll encounter.
Let’s start with the basics: bones are living, dynamic tissues. They’re constantly being broken down and rebuilt in a process called remodelling. This isn’t just maintenance—it’s adaptation. Bones respond to mechanical stress, repair microscopic damage, and help regulate calcium levels in the blood. But how does this happen? And what affects the bone’s ability to heal after injury?
Friday, 8 August 2025
Structure and Function of CNS Motor and Sensory Tracts 🧠
👋 Ready to dive into the highways of the nervous system? Buckle up, because today we’re exploring the Structure and Function of CNS Motor and Sensory Tracts! 💨
Tuesday, 5 August 2025
Stroke: Risk Factors, Epidemiology 🧠
Let’s dive deeper into stroke — a major global health burden and one of the leading causes of death and disability. Its impact spans acute care, rehabilitation, and long-term health outcomes, making it a cornerstone topic in medical education and public health.
Understanding the epidemiology, risk factors, and pathophysiology of stroke is essential not only for diagnosis and treatment but also for effective prevention strategies. Stroke is not a single disease but a spectrum of vascular events with diverse presentations, underlying mechanisms, and prognoses.
Here’s a structured breakdown to guide your understanding:• Stroke affects over 15 million people annually worldwide, with rising incidence in low- and middle-income countries.• In Australia, stroke is a leading cause of adult disability, with over 400,000 people living with its effects.• Ischaemic strokes account for ~85% of cases, while haemorrhagic strokes (intracerebral and subarachnoid) make up the remainder.• Age is the strongest predictor: risk doubles with each decade after 55.• Rural and remote populations often face delayed access to acute stroke care and rehabilitation services, contributing to worse outcomes.
Read on for risk factors and more !
Part 2: Brain Blood Supply – Clinical Correlations & Stroke Syndromes!
Now that you’ve explored the intricate anatomy of the brain’s blood supply — from the Circle of Willis to the branching cerebral arteries — it’s time to connect that knowledge to clinical practice. Understanding which regions are perfused by each artery allows you to localise neurological deficits with precision, especially in acute stroke presentations.
Monday, 4 August 2025
Clinical Presentation of Stroke: Pathophysiology & Key Differences 🧠💥
Stroke is one of the leading causes of death and disability worldwide — a true medical emergency where every minute counts. Whether due to vascular occlusion or haemorrhage, the resulting neurological injury demands timely intervention and a solid understanding of underlying mechanisms.
Part 1: Brain Blood Supply – The Anatomy Behind the Magic! 🧠
Today we’re exploring the vascular anatomy of the brain—because the brain may run the show, but without blood, it’s lights out! 💡
Here’s some basics
Wednesday, 30 July 2025
🧠 Seeing the Brain in Action: A Beginner’s Guide to Neuroimaging
You’ve learned to listen to the brain’s electrical activity with EEG — now it’s time to see it. Neuroimaging gives us a window into the brain’s structure, guiding diagnosis, understanding, and treatment.
But no single scan tells the full story. Each modality sees the brain differently — some reveal anatomy, others show activity — and choosing the right one means knowing what you’re asking, and what the scan can answer. This is just a primer to get you started - imaging is a long journey of learning to come !
Grant success: future AI symposium
I am very pleased to be part of the cross-institutional team that will be delivering a symposium
"Harnessing AI and technology for equitable and ethical medical education"
thanks to our successful GEMPASS Professional Development Education Grant.
Congratulations to the whole grant team - my collaborators from Macquarie University, Melbourne University, Deakin University and the University of Notre Dame - on our grant success. Looking forward to getting this work underway !!
- 📝 All posts about research and data →
- 📝 Identifying ideal applicants for medicine (2022) →
- 📝 Should we extend the currency of cognitive ability testing scores? (2023) →
- 📝 Automated protocol for assessing career rurality outcomes (2023) →
- 📝 Comparing rural and specialty choices of UOW graduates (2023) →
- 📝 Australian health workforce insights (2024) →
- 📝 Medical school admissions processes to target rural applicants (2025) →
Tuesday, 29 July 2025
🧠 How Do We Listen to the Brain? A Beginner’s Guide to EEG
Electroencephalography (EEG) is like eavesdropping on a conversation happening in your cerebral cortex. But instead of words, it uses electrical signals—and the patterns those signals make can tell us a lot about how the brain is functioning… or misfiring.
This post will outline the major important features of the EEG and how it can help us to understand the function, and dysfunction, of the brain.
Sunday, 27 July 2025
💊 Neurotransmitters on drugs: How alcohol, medications & other substances affect the CNS
Every action in the brain - whether catching a ball, calming a panic attack, or waking from anaesthesia - starts at the synapse. In physiology, you’ve already met the major neurotransmitters: GABA, glutamate, dopamine, serotonin, acetylcholine, and noradrenaline.
Now it’s time to see these in clinical action. If you haven't already read it, go back and check out the Neurotransmitters 101 post, it will help it all make sense.
Many drugs and substances - from prescription medications to recreational drugs - alter the brain’s electrochemical balance. They dial neurotransmitter signalling up or down, leading to effects that are therapeutic, recreational, harmful, or all three. Understanding how they work builds your clinical intuition - and helps you spot mechanisms behind both therapeutic effects and side effects.
We’ll explore how each class works, what effects they trigger, and where they act in the neural circuit. Consider this your pharmacological map of the CNS - designed for clarity, clinical context, and curiosity.
Saturday, 26 July 2025
🧠 Principles of Seizure Management
Seizures are a common clinical presentation—but behind each episode lies a nuanced web of causes, classifications, and considerations. Effective care begins with pattern recognition, cause exploration, and clinical prioritisation.
This guide walks through how clinicians approach seizure care—from the first event to long-term planning—by connecting symptoms to anatomy, treatment, and safety.
Clinical Cases in Seizure Localisation
Recognising seizure types isn't just about memorising lists — it's about observing patterns, interpreting subtle clues, and linking symptoms to functional neuroanatomy. The ability to reason clinically, even from brief descriptions, is one of the most important skills you’ll develop as a future doctor.
In this post, we’ll walk through a series of realistic case vignettes that should be a challenge for not just first years, but clinical second and third years as well.
Take your time with each one — some may seem straightforward, others more ambiguous. That’s okay. Clinical reasoning is a skill, not an instinct — and every case you puzzle through builds it.
Friday, 25 July 2025
To Anki or not to Anki: Why flashcards aren’t the whole story in medical education
Flashcards have become the unofficial religion of medical study.
🧠 Anki isn’t evil - but it’s also not enough
And sometimes, it might be the very thing slowing you down.
🌐 Navigating the blog: A guide to getting the most out of it
Welcome! Whether you’ve stumbled in while revising neuroanatomy or you're deep in a diagnostic reasoning rabbit hole, this blog was designed to help you connect clinical concepts, and spark questions that actually matter.
It's a scaffolded learning tool designed to provoke thinking, support understanding, and build clinical intuition. Here’s how to dive deeper and make the most of it.
🧠 CONSCIOUSNESS (and how we can lose it)
Consciousness might seem like something “obvious”—you know when you’re awake, alert, and aware. But understanding what consciousness is (from a medical perspective), and why it can be disrupted, is fundamental to learning clinical neurology and emergency medicine. Let’s build the foundation.
Thursday, 24 July 2025
🧠 NEUROTRANSMITTERS 101: The Basics of Neurotransmission
Ready to dive into the fascinating world of neurotransmitters? These tiny molecules are the chemical messengers that keep your nervous system humming—coordinating thoughts, movements, moods, and memories.
Let’s explore how these molecules work and why they’re clinically meaningful. 🩺
Tuesday, 22 July 2025
Localisation of seizures 🧠
When someone has a seizure, the symptoms can tell us more than just what happened — they give clues about where in the brain it happened. Seizure localisation is the art and science of mapping signs and behaviours to specific cortical regions. From staring spells to sudden muscle jerks, each presentation points to a unique neural epicentre.
Understanding where seizures begin helps us decode the circuitry behind them, guides diagnosis, and even shapes treatment decisions. Let’s explore how brain geography becomes clinical insight.
Understanding Seizure Classification 🧠
Hey future doctors! 👋 Let's dive into the fascinating world of seizure classification. 🩺✨
🔬 Pathophysiology of Seizures: What’s Going Wrong?
Seizures are caused by abnormal, excessive, synchronous electrical activity in groups of neurons. Seizures are like a power surge in the brain. Instead of orderly, purposeful neural signals, you get a storm of chaotic, excessive firing across neuron groups.
This hyperactivity disrupts normal function — from movement and sensation to awareness and behaviour.
Monday, 21 July 2025
🧠 From Cortex to Brainstem: Mapping the Machinery of Thought and Function
The central nervous system (CNS) isn’t just a bundle of grey and white matter—it’s the command centre for sensation, movement, cognition, and survival. Understanding its architecture sets the stage for recognising how neurological damage unfolds in real patients.
Let’s take a tour through the cortex, subcortex, and brainstem—with just enough anatomical and functional depth to make it stick.
Wednesday, 25 June 2025
🩺 When the Filters Fail: A review of reduced renal function
👩⚕️ Meet Karen, a 54-year-old woman with Type 2 Diabetes and longstanding hypertension. She’s noticed some ankle swelling, increasing fatigue, and mild nausea. Her GP runs bloods— her eGFR is 38 mL/min/1.73m², her creatinine is up, and there’s proteinuria.
Beneath those swelling ankles lies a story of pressure, filtration failure, and systemic fallout. This is where physiology meets clinical reality, and small changes start to snowball.
🧠 Interpreting Renal Function Tests:
Renal function tests aren’t just numbers — they’re clues. When interpreted thoughtfully, they can help us distinguish between dehydration, intrinsic renal disease, and post-renal obstruction. In this post, you’ll meet patients like Tom, who presents with dehydration and rising creatinine; Aisha, whose frothy urine holds a glomerular secret; and Leo, whose “normal” labs conceal a chronic decline — all to help you decode renal results with clinical confidence.
We’ll explore how to interpret renal function tests and urinalysis through a clinical reasoning lens — breaking down key blood and urine markers, comparing patterns across different types of kidney injury, and working through real-world cases to bring the concepts to life.

























.jpeg)






















