Infections in the renal system are among the most common reasons patients present to GPs and emergency departments — yet their underlying mechanisms are often oversimplified. These aren't just “bladder bugs” causing discomfort: they are dynamic, evolving conditions that reflect an interplay between microbial virulence, host defence, and anatomical vulnerabilities.
From the relatively straightforward presentation of cystitis to the more serious implications of pyelonephritis, renal infections provide a perfect lens through which to explore the clinical relevance of physiology and pathophysiology. How does a bacterium from the gut end up damaging a kidney? What determines whether a simple UTI becomes a systemic illness? And how do we decide when antibiotics, imaging, or hospital admission are truly necessary?
In this post, we’ll explore how renal infections arise, what differentiates upper from lower tract involvement, and how pathophysiological principles guide investigation and treatment decisions.
1 1. The Spectrum: From Cystitis to Pyelonephritis
Urinary tract infections (UTIs)
are often discussed as a single entity, but they actually represent a spectrum
of disease — from localised irritation of the bladder to more serious
infections involving the kidneys. Understanding where the infection sits
helps explain how it presents and why it matters.
💡 Lower Urinary Tract Infection (Cystitis)
When infection remains confined to the bladder, it typically causes:
- Dysuria
(pain or burning on urination)
- Frequency
and urgency, due to inflammation of the bladder wall
- Suprapubic
discomfort, often described as a pressure or heaviness
- Haematuria-
either macroscopic (visible blood) or microscopic, picked up on
dipstick or microscopy
- No
systemic features — the patient usually feels otherwise well
This is the classic “uncomplicated
UTI,” most commonly seen in healthy women.
🔺 Upper Urinary Tract Infection (Pyelonephritis)
If bacteria ascend via the ureters
and reach the renal pelvis or parenchyma, the infection becomes more serious.
The clinical picture shifts to include:
- Fever,
often with rigors
- Flank
or loin pain, due to inflammation around the kidney
- Nausea
or vomiting, reflecting systemic illness
- Sometimes
lower tract symptoms, but not always
The infection now involves a
well-perfused organ — the kidney — making bacteraemia and sepsis more
likely if left untreated. This is why pyelonephritis warrants early recognition
and prompt management.
|
Site |
Typical Features |
|
Lower urinary tract (e.g. cystitis) |
Dysuria, frequency, urgency, suprapubic discomfort. Systemically
well. |
|
Upper urinary tract (e.g. pyelonephritis) |
Fever, loin or flank pain, nausea/vomiting, systemic signs. ± Lower
tract symptoms. |
2. Host Defence and Renal Vulnerability
Despite being connected to the
outside world, the urinary tract is remarkably good at defending itself from
infection. In fact, most people produce litres of urine every day without ever
developing a UTI. That’s thanks to a combination of mechanical flushing,
chemical composition, anatomical barriers, and immune vigilance.
🧪 Natural Defences
- Urine
is not a welcoming place for bacteria: it's slightly acidic, has a
high urea concentration, and lacks nutrients. These properties inhibit
bacterial growth.
- Regular
voiding flushes pathogens from the bladder before they can adhere to
the urothelium and colonise.
- Urothelial
cells express antimicrobial peptides and can initiate immune responses
when invaded.
But as robust as this system is,
it's not infallible — and several factors can tip the balance in favour of
infection.
🛠️ Anatomical and Mechanical Factors
- The
female urethra is short and closer to the anus, making it easier
for enteric bacteria (like E. coli) to access the bladder. This
explains why UTIs are significantly more common in women.
- Catheterisation
bypasses the urethral defence entirely, creating a direct path for
bacteria to ascend and form biofilms.
- Vesicoureteric
reflux (VUR) — a condition where urine flows backward from the bladder
into the ureters — can carry bacteria up into the kidneys. VUR is
particularly relevant in children with recurrent UTIs.
- Urinary
tract obstruction (e.g. due to stones, strictures, or enlarged
prostate) leads to stasis — and stagnant urine is a prime breeding ground
for infection.
🌡️ Systemic Host Factors
Certain physiological or disease
states reduce resistance to infection:
- Pregnancy
leads to dilated ureters and reduced bladder tone, promoting stasis and
increasing the risk of pyelonephritis.
- Diabetes
mellitus impairs immune responses and may cause glycosuria, creating
an inviting environment for bacterial growth.
- Immunosuppression, whether due to medications or conditions like HIV, weakens the body's ability to contain infection once it begins.
🧠 Takeaway: The
urinary tract has robust defences, but infections occur when bacteria either
bypass those barriers or the host is unable to mount an adequate response.
Knowing who is at risk — and why — is key to early recognition and appropriate
management.
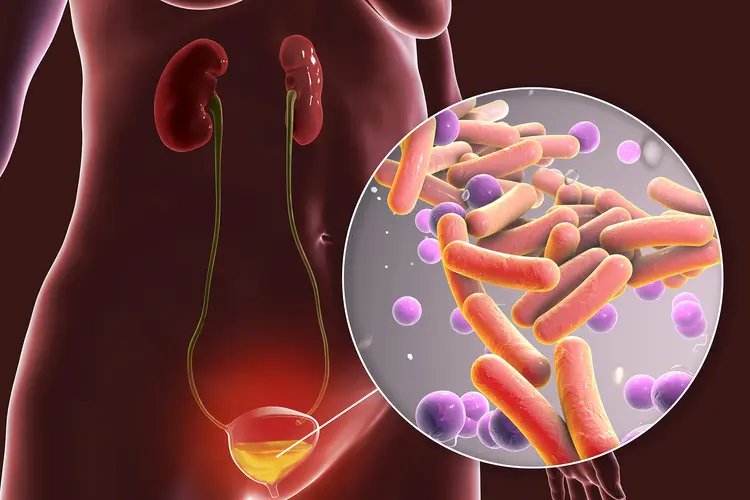
3. Uropathogens: Not Just a List
Many urinary tract infections are
caused by a familiar cast of bacteria, but what makes one organism succeed
where others don’t? To understand clinical patterns — who gets sick, how they
present, and why some infections persist — it’s worth exploring the microbes
through the lens of colonisation, adhesion, and immune evasion.
💩 Escherichia coli: The Opportunistic Local
E. coli causes about 75–90%
of community-acquired UTIs — but it’s not just there by chance. This
gut-dwelling Gram-negative rod possesses a series of tools that help it survive
and thrive in the urinary tract:
- Adhesins
(like P fimbriae) allow E. coli to latch onto uroepithelial cells
and resist the flushing effects of urine.
- Type
I fimbriae mediate initial bladder colonisation, while P fimbriae
are associated with pyelonephritis.
- It
can form biofilms on uroepithelium or catheters, allowing
persistence and resistance to immune clearance.
- Some
strains have capsules that block phagocytosis and reduce immune
detection.
🧠 Takeaway: The
dominance of E. coli isn’t accidental — it reflects its evolved ability
to bind, hide, and persist in a hostile environment.
🦠 Klebsiella & Proteus: The Opportunists
These Gram-negative rods are less
common in uncomplicated UTIs but become more prominent in:
- Recurrent
infections
- Structural
abnormalities
- Urinary
stasis or obstruction
🧠 Clinical clue: A
patient with recurrent UTIs, alkaline urine, and staghorn calculi? Think
Proteus.
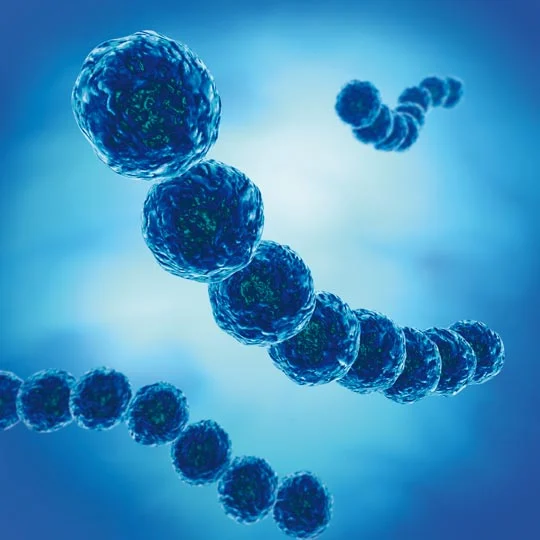
🧫 Enterococcus: The Catheter Survivor
This Gram-positive cocci is part of normal gut flora but becomes more relevant in:- Hospital-acquired
UTIs
- Catheter-associated
infections
- Immunocompromised
hosts
🧠 Clinical point:
Not all urinary bugs are Gram-negative — Gram-positives like Enterococcus
signal a shift in setting, risk factors, or equipment.
🌸 Staphylococcus saprophyticus: The Specialist
While often overlooked, S.
saprophyticus is a coagulase-negative staph that specifically
affects:
- Young,
sexually active women
- Often
causes acute uncomplicated cystitis
- Lacks
dramatic virulence, but adheres well to urothelium and often escapes
immune clearance without systemic signs
🧠 Pearl: In young
women with cystitis but negative nitrites on dipstick, S. saprophyticus
is a common culprit — it doesn’t reduce nitrates like E. coli does.
|
Common Organisms |
Comments |
|
Escherichia coli |
Most common (esp. community-acquired); faecal origin |
|
Klebsiella, Proteus |
More common in recurrent or structural abnormality |
|
Enterococcus |
Often hospital-acquired or catheter-related |
|
Staphylococcus saprophyticus |
Seen in young, sexually active females |
🦠 Proteus species
can alkalinise urine → predispose to struvite stones
🧠 Thinking Beyond the Bladder: When UTI Isn’t So Simple
Before diving into treatment,
especially in patients with recurrent UTIs or unusual symptoms, take a step
back and ask:
- Is
there an anatomical cause?
Think obstruction (e.g. stone, stricture), reflux, incomplete emptying — any factor that impairs normal urine flow can create a breeding ground for infection. - Is
this truly a UTI?
Not all dysuria is infectious. Consider STIs, vaginal atrophy, or interstitial cystitis — especially if there’s sterile pyuria or treatment failure. - Are
they responding to treatment as expected?
If symptoms persist beyond 48–72 hours or recur soon after antibiotics, investigate further: wrong bug? Wrong drug? Or a deeper problem?
While most UTIs are straightforward, not all that burns is
cystitis, and not all infection is simple.
|
Flag |
Consider |
|
Male patient with UTI |
Investigate for urinary obstruction, prostatitis, or structural
abnormality |
|
Sterile pyuria (white cells but no bacteria) |
STI, interstitial cystitis, renal TB (rare), contamination |
|
Recurrent infections |
Reflux, stones, incomplete bladder emptying, diabetes |
|
No improvement after 48–72 hours |
Resistant organism, incorrect diagnosis, renal involvement |
|
Atypical symptoms (e.g. flank mass, persistent fever) |
Obstruction, abscess, or alternative pathology (e.g. malignancy) |
🧠 Tip for students:
Any time something feels “off-script” in a UTI presentation, pause and ask — is
this a red flag, or just a variation on the usual
4. Management Principles
When it comes to urinary tract
infections, effective management begins with recognising where the
infection is, how sick the patient is, and what host factors
might complicate its course. Diagnosis and treatment decisions are rooted in
understanding the bacterial burden, the host’s defences, and the risk of
progression.
🧪 Diagnosis
Urinalysis is the
first-line tool for bedside diagnosis:
- Leukocytes
(white blood cells) suggest inflammatory response in the urinary tract.
- Nitrites
are formed when certain bacteria (notably E. coli) convert urinary
nitrates — a useful indirect marker of Gram-negative infection.
- Microscopic
or macroscopic haematuria may reflect urothelial irritation,
particularly in cystitis.
These clues help identify
infection but do not replace clinical judgement — especially in older patients
or those with atypical presentations.
Urine culture becomes
essential when:
- The
patient is systemically unwell (e.g. pyelonephritis)
- The
presentation is atypical, recurrent, or in men (who
typically don’t get UTIs unless something else is going on)
- There's
concern for antibiotic resistance (e.g. recent hospitalisation or
travel, or prior resistant organisms)
- You’re
not sure if it’s truly a UTI or another condition mimicking
symptoms
Cultures confirm the organism and
its sensitivities — critical for tailoring therapy in complicated cases.
💊 Pharmacological Management:
The right drug, for the right bug, in the right tissue — at the right time.
Uncomplicated Cystitis (in nonpregnant adults)
- Generally
treated empirically with a short course of oral antibiotics (e.g. trimethoprim,
nitrofurantoin)
- Rationale:
These patients are systemically well, the likely pathogen is predictable (E.
coli), and the infection is localised.
First-line options (per eTG):
- Trimethoprim 300 mg orally, daily for 3
days
- Nitrofurantoin 100 mg orally, every 6
hours for 5 days
Why these?
- Both are narrow-spectrum
agents that concentrate well in the bladder.
- Despite 20% resistance to
trimethoprim in E. coli, it's still first-line because treatment
failure in otherwise well patients is uncommon — and the broader aim is to
avoid unnecessary use of broader-spectrum agents.
- Nitrofurantoin remains
effective but depends on adequate renal function (eGFR >30 mL/min) to
concentrate in the urine.
When to avoid:
- Nitrofurantoin should not
be used for suspected pyelonephritis — it doesn’t reach renal
tissue at therapeutic levels.
- Always review allergies and
potential for pregnancy.
Pyelonephritis: Depth of Infection, Depth of Treatment
· Rationale: Prompt bactericidal treatment reduces risk of bacteraemia, sepsis, and permanent renal damage.
|
Clinical status |
Recommended empirical
treatment |
Why this choice? |
|
Mild/moderate, systemically well |
Oral amoxicillin + clavulanate |
Good oral bioavailability and
tissue penetration; covers E. coli and other Gram-negatives |
|
Penicillin allergy (non-severe) |
Oral ciprofloxacin |
Excellent renal penetration;
used cautiously due to risk of resistance and collateral damage |
|
Systemically unwell (fever
≥38°C, vomiting, sepsis) |
IV gentamicin plus IV
amoxicillin or ampicillin |
Gentamicin provides broad
Gram-negative coverage; amoxicillin adds Enterococcus and
Gram-positive coverage. Rapid IV delivery matches the clinical urgency. |
🧠
Why not nitrofurantoin or fosfomycin?
These drugs do not achieve adequate concentrations in kidney tissue and are not
appropriate for infections above the bladder.
💡
First-year insight: We choose antibiotics based not just on the bug, but
on the depth of infection, the tissue involved, and the risk
of deterioration. A cystitis can fail to improve with trimethoprim, and
that’s okay — but starting the wrong agent in pyelonephritis can delay
clearance, allow sepsis, and harm the kidney itself.
Warnings
- Many
antimicrobials are renally excreted or nephrotoxic at high doses.
- Always check renal function before prescribing — particularly for aminoglycosides (eg gentamycin), which are effective but potentially nephrotoxic
Gentamicin is a potent aminoglycoside antibiotic often used in severe pyelonephritis. It’s rapidly bactericidal against Gram-negative organisms like E. coli and concentrates well in renal tissue — exactly what’s needed in serious kidney infections.
But there’s a catch:
- Gentamicin is nephrotoxic and ototoxic, particularly when:
- Dosed incorrectly
- Given for prolonged periods
- Used in patients with impaired renal function or volume depletion
📚 First-year insight: Aminoglycosides are lifesaving in the right context — but like many powerful tools, they demand respect and close monitoring.
⚠️ Recognise Red Flags
Certain features suggest the
infection is no longer confined to the urinary tract:
- Persistent
vomiting → can’t absorb oral meds
- Rising
creatinine → may indicate urosepsis or obstructive uropathy
- Hypotension,
tachycardia, or rigors → systemic inflammatory response
- Flank
pain worsening despite treatment → consider abscess or obstruction
🧠 These patients need
escalation — often to hospital care for IV fluids, imaging, and close
monitoring.
💧 Non-Pharmacological Management: Supporting the System
While antibiotics are the
cornerstone of treatment, several supportive measures can ease symptoms,
promote recovery, and reduce recurrence — especially in uncomplicated lower
UTIs.
🥤 Fluids
- Encouraging
adequate hydration helps dilute urine and promotes frequent voiding,
which can mechanically flush bacteria from the bladder.
- There’s
no magic volume, but aiming for clear or pale yellow urine is a
practical guide.
- In
pyelonephritis or systemic illness, IV fluids may be needed to
support perfusion and renal function.
🧠 Caution:
Overhydration doesn’t “cure” infection and may worsen hyponatraemia in
vulnerable patients — especially the elderly.
💊 Pain Relief: Targeting Inflammation
- Paracetamol
is first-line for dysuria and suprapubic discomfort.
- NSAIDs
(e.g. ibuprofen) may help with inflammation and fever, but use with
caution in patients with impaired renal function or dehydration.
- Phenazopyridine
(not widely used in Australia) is a urinary tract analgesic that can
relieve dysuria but may mask worsening symptoms.
NSAIDs (like ibuprofen) are helpful for fever and dysuria in UTIs — but they reduce prostaglandin synthesis, which in turn decreases afferent arteriole dilation.
- In healthy people, NSAIDs are usually well tolerated
- But in someone who’s volume-depleted (e.g. due to fever, vomiting, pyelonephritis), NSAIDs may reduce renal perfusion and cause acute kidney injury
- Risk is highest in the “triple whammy” of NSAID + ACE inhibitor + diuretic
🧪 Urinary Alkalisers:
Comfort, Not Cure
- Products
like sodium citrate or potassium citrate can reduce urinary
acidity, which may ease dysuria.
- They
do not treat infection and should be used as adjuncts only.
- Avoid
in patients with renal impairment or those on sodium-restricted diets.
🍒 Cranberry Products:
Prevention, Not Treatment
Cranberries have long been
promoted for UTI prevention — but what does the evidence say?
A 2023 Cochrane
review found that cranberry juice or supplements can reduce the risk of
recurrent UTIs in women, children, and people at higher risk (e.g.
post-catheterisation). The proposed mechanism is that proanthocyanidins
in cranberries inhibit E. coli from adhering to the bladder wall.
- The
benefit is preventive, not therapeutic — cranberry products do
not treat active infections.
- There’s
no proven benefit in elderly patients, pregnant women, or those
with incomplete bladder emptying.
- Products
vary in concentration and formulation, making dosing inconsistent.
🧠 Bottom line: Cranberry may help reduce recurrence in select groups, but it’s not a substitute for antibiotics when infection is present. It is harmless however, and if it encourages people to drink more fluids then that alone may help infection.
Nitrofurantoin works best in acidic urine (low pH).
Urinary alkalinisers (like Ural, Citravescent, or potassium citrate) raise urinary pH, making the environment less favourable for nitrofurantoin and potentially reducing its effectiveness.
🧠 Takeaway: If a patient is prescribed nitrofurantoin, avoid using urinary alkalisers during the same treatment course — reach for paracetamol instead for dysuria relief.
🩺 Clinical Case: A Chilling Flank
A 36-year-old woman presents with
2 days of fever, rigors, left flank pain, and nausea. She also reports urinary
frequency and dysuria. On examination, her temperature is 38.9°C and there’s
tenderness over her left costovertebral angle. Her BP is 106/64 mmHg, HR 102
bpm.
Urinalysis:
- Positive
for leukocytes and nitrites
- Moderate
haematuria
Blood tests:
- WCC:
14.2 ×10⁹/L (↑)
- Creatinine:
98 µmol/L (normal)
- CRP:
180 mg/L (↑)
She is diagnosed with acute
pyelonephritis and started on intravenous ceftriaxone.
🧠 Reflection questions
- What clues point toward an upper tract infection in this patient?
- Why is a urine culture important in this case?
- What host factors may increase the risk of progression from lower to upper tract infection?
· Anatomical issues like vesicoureteric
reflux or obstruction (e.g. stone, tumour, or enlarged prostate)
·
Immunosuppression, whether due to disease
or therapy, weakens systemic response to early infection
·
Pregnancy alters ureteral tone and flow,
promoting stasis
·
Delays in diagnosis or treatment allow
organisms to multiply and ascend unchallenged
🧠
In this patient’s case, even without comorbidities, a short delay in seeking
care may have allowed progression — a reminder that host vulnerability is often
dynamic, not fixed
- Why start with IV antibiotics?
⏭️ What Next? Monitoring and Moving Forward
Once a patient with pyelonephritis
is started on IV antibiotics, management decisions don’t stop — they evolve.
Here's how to think about the next steps:
🧪 1. Review Culture Results
- Tailor
antibiotics based on sensitivity patterns — especially if initial
therapy was empirical.
- If
E. coli is confirmed and sensitive to oral agents, consider stepping
down to oral therapy once the patient improves clinically (afebrile,
tolerating fluids, stable vitals).
💊 2. Step Down (When Ready)
- Patients
can be switched to oral antibiotics once they:
- Have
been afebrile for at least 24 hours
- Can
tolerate oral intake
- Are clinically improving
- Total
duration is usually 10–14 days, including both IV and oral phases.
🧠 3. Ask Why It Happened
Even if the episode resolves,
always ask:
- Was
there a delay in presentation or diagnosis?
- Is
this a first-time infection, or are there signs of recurrence?
- Could
pregnancy, diabetes, obstruction, or reflux be contributing?
- Should
the patient have a renal ultrasound, particularly if not improving,
or if this isn’t their first episode?
📆 4. Plan Follow-Up
- Organise
GP review post-discharge with culture results and antibiotic plan.
- For
recurrent infections or unclear cause, consider referral for urological
imaging or specialist input.
🧠 Final pearl:
Management doesn’t stop at symptom resolution — it’s also about making sure
this doesn’t happen again, and knowing when an “ordinary UTI” might be masking
something more.
🔁 Reflection Prompts: Sense-Making, Not Memorising
Use these to test your clinical
reasoning — not just whether you know the facts, but whether you understand why
they matter.
- How
does the presentation of pyelonephritis differ from cystitis — and what
does this tell you about the depth of infection?
- Why
might patients with diabetes or pregnancy be more vulnerable to ascending
renal infections?
- How
does the body attempt to defend against urinary tract infections — and
what factors can overcome these defences?
- What
are the risks of delaying appropriate treatment in upper UTIs?
- How
do you match the severity of illness to your route and choice of
antibiotics?
🧠 Tip: If you can
talk through these aloud or teach them to a peer, you're not just learning —
you're building your diagnostic intuition.
🧵 Wrapping It Up: Beyond Bugs and Drugs
Urinary tract infections might
seem simple — common, familiar, easily treated. But as you’ve now seen, they
offer a rich chance to practise thinking like a clinician:
- To
ask not just what the diagnosis is, but why this patient got
sick at this moment
- To
choose treatment that’s not just “by the book,” but right for this
tissue, this bug, and this host
- To
recognise that sometimes, what looks like a UTI is actually something
more — or something different
Whether it’s understanding why
nitrofurantoin won’t work in pyelonephritis, spotting sterile pyuria in an STI,
or matching IV therapy to systemic signs — the goal isn’t just to memorise
facts. It’s to build a habit of clear, conscious clinical reasoning that
flexes with context.















No comments:
Post a Comment