🩸 Nephritic vs Nephrotic Syndrome: Clinical Clues from a Leaky Filter
Nephritic syndrome is driven by inflammation — red cell casts, haematuria, and oliguria often dominate.
Nephrotic syndrome is driven by barrier dysfunction — marked proteinuria, hypoalbuminemia, and oedema take centre stage.
We’ll discuss:
- The pathophysiologic logic behind each
- How different GN types map onto this spectrum
- Real cases with investigation findings and reasoning prompts
🔍 1: What Is Nephritic Syndrome?
- Mechanism: Immune-mediated inflammation → capillary wall damage → haematuria ± mild proteinuria
- Key features: Haematuria, red cell casts, hypertension, oliguria, mild-moderate proteinuria
- Examples: PSGN, IgA nephropathy, lupus nephritis (Class III/IV), anti-GBM disease
🧠 Clinical analogy: The filter is red, swollen, and angry — it still filters, but leaks blood and resists flow.
🩸 Nephritic Syndrome: When the Filter Is Angry
Nephritic syndrome refers to a clinical picture caused by inflammatory damage to the glomerular capillary wall. The injury typically affects the endothelium and mesangium, triggering a brisk immune response that impairs filtration and allows red blood cells and some protein to leak into the urine.
🔍 Core Mechanism
At the root is immune-mediated inflammation — often with neutrophil recruitment — which:
- Narrows or obstructs glomerular capillaries → reduced glomerular filtration rate (GFR)
- Damages the filtration barrier → haematuria, often with red cell casts
- Disrupts vascular autoregulation → salt and water retention, contributing to hypertension and oedema
This inflammation may be triggered by:
- Immune complex deposition (e.g. PSGN, IgA nephropathy)
- Autoantibodies (e.g. anti-GBM)
- Neutrophil activation (e.g. ANCA vasculitis)
🔑 Key Clinical Features
- Haematuria: often visible ("tea-coloured" or "cola-coloured" urine)
- Red cell casts: shaped by tubules, indicating glomerular bleeding
- Proteinuria: usually mild to moderate
- Hypertension: due to salt retention and RAAS activation
- Oliguria: reflecting reduced GFR
- ± Oedema: often periorbital or dependent
🧠 What’s Happening in the Filter?
Think of the glomerulus as a sieve. In nephritic syndrome, the sieve is inflamed, swollen, and clogged — so it filters poorly and leaks blood. It’s like trying to force water through a sponge: pressure builds, flow slows, and what's coming out isn’t clean.
🩺 Case Example: Nephritic Syndrome (Post-Infectious GN)
History:
A 9-year-old boy presents with facial puffiness and dark brown urine for the past two days. His parents report that he had a sore throat about two weeks ago but didn’t see a doctor. He now appears slightly lethargic and complains of vague abdominal discomfort.
Examination findings:
- Mild periorbital and pedal oedema
- Blood pressure: 135/90 mmHg
- No rash, joint pain, or lung findings
Investigations:
- Urinalysis: red cell casts, mild proteinuria
- Serum creatinine: mildly elevated
- C3: low
- ASO titre: elevated
- What syndrome does this presentation suggest?
- How does the timing of the sore throat relate to the current symptoms?
- Which features help you distinguish this from nephrotic syndrome?
🧪 Diagnosis: Post-streptococcal glomerulonephritis (a classic nephritic syndrome)
This case illustrates immune complex–mediated inflammation of the glomerulus, with low complement, haematuria, and mild proteinuria, all emerging days to weeks after streptococcal infection.
🤓 Why These Findings?
In post-streptococcal glomerulonephritis, circulating immune complexes deposit in the glomeruli and activate complement, particularly the alternative pathway. This leads to an influx of neutrophils and inflammation, damaging the glomerular capillary walls.
- Haematuria occurs because red blood cells escape through the compromised filtration barrier, often forming red cell casts as they mould in the tubules.
- Mild proteinuria reflects limited podocyte injury — enough to leak some protein, but not to the degree seen in nephrotic syndrome.
- Low C3 levels reflect complement consumption during immune activation,
- raised ASO titre confirms recent streptococcal exposure.
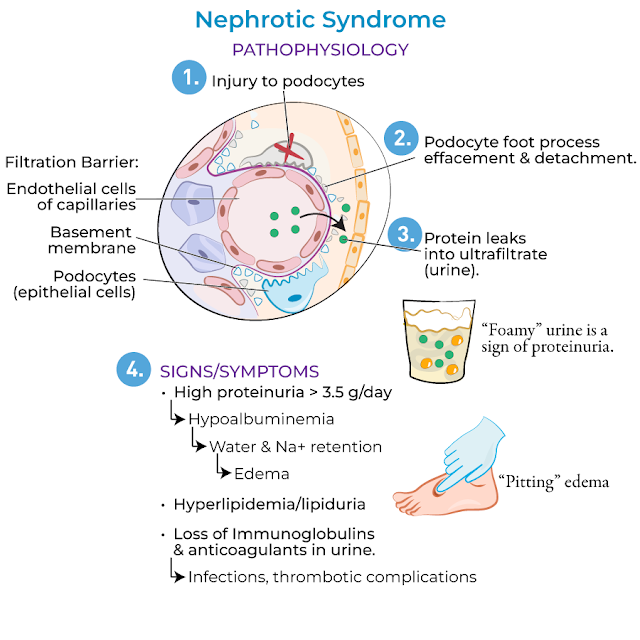
💧 2: What Is Nephrotic Syndrome?
- Mechanism: Podocyte and slit diaphragm dysfunction → massive protein leak
- Key features: Proteinuria >3.5g/day, hypoalbuminemia, edema, hyperlipidemia
- Examples: Minimal change disease, membranous nephropathy, FSGS, lupus nephritis (Class V)
🧠 Clinical analogy: The filter is punched full of holes — blood cells may stay in, but protein pours out.
💧 Nephrotic Syndrome: When the Filter Becomes a Sieve
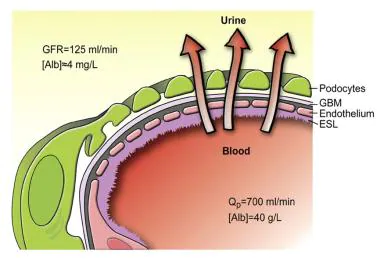
Nephrotic syndrome refers to a constellation of signs driven by excessive protein loss in the urine, typically due to damage to podocytes and the glomerular filtration barrier. Unlike nephritic syndrome, the process here is usually non-inflammatory — the capillary wall isn’t inflamed, it’s structurally compromised.
🔍 Core Mechanism
The main issue is podocyte injury or dysfunction — either via direct toxin, immune-mediated damage, or structural disruption — which leads to:
- Loss of slit diaphragm integrity
- Increased permeability of the basement membrane to large proteins, especially albumin
- Resultant hypoalbuminaemia, triggering hepatic synthesis of lipids and activation of sodium-retaining systems
🔑 Key Clinical Features
- Heavy proteinuria: often >3.5 g/day
- Hypoalbuminaemia: due to urinary albumin loss
- Oedema: generalised (“anasarca”), sometimes periorbital or sacral
- Hyperlipidaemia and lipiduria: due to hepatic overcompensation
- Normal or slightly elevated blood pressure
- Urinary casts: may show “fatty casts” with a Maltese cross appearance under polarised light
🧠 What’s Happening in the Filter?
Think of the glomerulus as a finely woven net. In nephrotic syndrome, the holes in that net have been stretched or torn — so large proteins like albumin fall through in large amounts. The body tries to compensate but can't keep up, and the result is swelling, low oncotic pressure, and secondary metabolic effects
🩺 Case Example: Nephrotic Syndrome (Minimal Change Disease)
History:
A 4-year-old boy is brought in with puffy eyelids and swelling in his lower limbs. His parents noticed that his clothes feel tight, and his urine looks frothy but otherwise normal. He has no fever or preceding illness.
Examination findings:
- Facial and lower limb oedema
- Normal blood pressure
- No rash, joint symptoms, or respiratory findings
Investigations:
- Urinalysis: 4+ protein, no red cells or casts
- Serum albumin: markedly reduced
- Cholesterol: elevated
- Renal function: normal
- Urine microscopy: oval fat bodies (“Maltese crosses”)
🤓 Why These Findings?
In minimal change disease — the most common cause of nephrotic syndrome in children — podocyte foot processes become effaced, but glomeruli appear largely normal under light microscopy. This structural disruption of the slit diaphragm allows unregulated protein loss. As albumin levels fall, plasma oncotic pressure decreases, leading to fluid shift into interstitial spaces and oedema. The liver responds with increased lipid production, explaining the hypercholesterolaemia and lipiduria. The absence of haematuria or hypertension supports a non-inflammatory, “nephrotic” process.
🧪 3: Comparing the Syndromes
|
Feature |
Nephritic
Syndrome |
Nephrotic
Syndrome |
|
Urine |
Haematuria ±
proteinuria |
Heavy
proteinuria (>3.5g/day) |
|
Casts |
Red cell
casts |
Fatty casts
("Maltese cross") |
|
Blood
pressure |
Often
elevated |
Often normal |
|
Oedema |
Mild or
periorbital |
Generalized,
marked |
|
Serum albumin |
Normal or
slightly reduced |
Low |
|
Cholesterol |
Usually
normal |
Elevated |
|
Complement |
May be low
(e.g. PSGN, lupus) |
Usually
normal (except lupus) |
These syndromes are not distinct diseases, but overlapping patterns that reflect the nature and location of glomerular injury. Recognising the dominant clinical features — haematuria or proteinuria, hypertension or hypoalbuminaemia — can guide the next steps in investigation and help narrow the diagnostic field
Here's a nice video I found on Youtube that gives a high level summary and comparison
- New onset haematuria (esp. cola-coloured)
- Proteinuria on dipstick
- Hypertension in a young patient
- Facial or peripheral oedema
- Reduced urine output
- Recent infection, autoimmune features, or systemic symptoms
🩺 Principles of Management in Glomerulonephritis
Management isn’t one-size-fits-all — it depends on the underlying cause, the clinical syndrome (nephritic vs nephrotic), and the severity of renal involvement. But the following principles offer a consistent scaffold:
1. Address the Underlying Cause
- Infection-related GN: Supportive care ± antibiotics (e.g. PSGN)
- Autoimmune GN: Immunosuppression (e.g. corticosteroids, cyclophosphamide, rituximab)
- ANCA vasculitis or anti-GBM disease: Often requires urgent immunosuppression ± plasmapheresis
2. Control Blood Pressure and Preserve Renal Function
- ACE inhibitors or ARBs: reduce intraglomerular pressure and proteinuria
- Target <130/80 mmHg in most patients
- Monitor renal function and potassium closely
3. Manage Oedema and Volume Status
- Salt restriction and loop diuretics (e.g. furosemide) for fluid overload
- Albumin infusions are generally reserved for severe hypoalbuminaemia with refractory oedema
4. Treat Proteinuria and Its Consequences
- ACEi/ARB also reduce protein loss in nephrotic-range cases
- Consider statins for marked hyperlipidaemia if persistent
5. Supportive Care and Monitoring
- Watch for AKI or rising creatinine → may need dialysis in severe cases
- Monitor urine output, weight, and electrolytes
- Refer to nephrology early — especially if rising creatinine, refractory hypertension, or RPGN
6. Biopsy When Diagnosis or Prognosis Is Unclear
- Biopsy guides classification, prognosis, and treatment decisions — particularly when serology is non-diagnostic or rapid progression is suspected








No comments:
Post a Comment